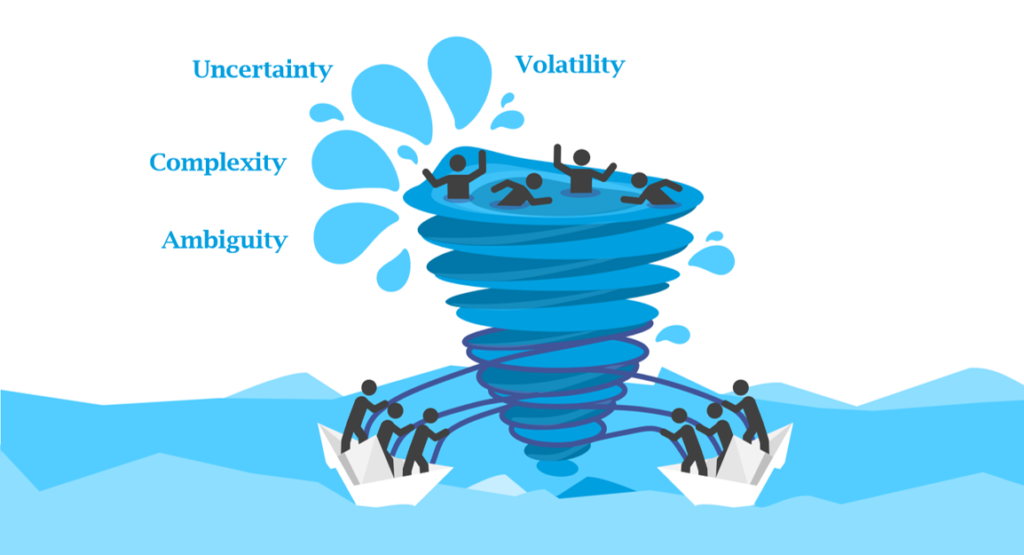
The healthcare landscape is a microcosm of the world – volatile, uncertain, complex, and ambiguous (VUCA). These VUCA elements challenge healthcare organizations, particularly those serving marginalized communities, in delivering equitable, quality care.
Ever-changing policies, disruptive innovations, and fluctuating funding scenarios exemplify volatility in healthcare. During the height of the tumultuous COVID-19 pandemic, healthcare leaders continuously adapted to new guidelines, managed sudden resource allocations, and facilitated urgent digital transitions. However, volatility is not limited to crises. Daily, healthcare organizations must navigate fluctuating supply costs, evolving patient demographics, and innovations in healthcare technologies. For example, the widespread adoption of artificial intelligence and machine learning in health analytics can drastically change the diagnostics landscape, providing opportunities for improvement and bringing fresh challenges in managing and regulating this new frontier.
Uncertainty, a close companion of volatility, is a steadfast fixture in healthcare. Leaders and providers must forecast disease outbreaks, anticipate patients’ needs, and align these with organizational goals. The advent and acceptance of telehealth, accelerated by the pandemic, has added another layer of uncertainty. While telehealth offers vast potential for reaching underserved populations and streamlining care, it also brings new challenges in regulations, patient privacy, and technology disparities among populations.
Complexity is a cornerstone of healthcare, inherent in varied clinical cases, intricate organizational structures, and emerging payment models. Chronic disease management underscores this complexity, requiring seamless coordination among healthcare professionals, treatment modalities, and various health and social determinants. A patient with diabetes, for example, may require the collaborative care of endocrinologists, dietitians, podiatrists, and social workers, in addition to monitoring various determinants like blood sugar levels, dietary habits, physical activities, and social support.
Ambiguity, the final element of the VUCA framework, is interwoven within healthcare’s fabric, creating uncertainties about the interpretation of information or the future direction of actions. Genetic testing, an emerging field in personalized medicine, epitomizes this ambiguity. The vast amount of data generated from genetic tests can suggest multiple intervention paths, making the decision-making process intricate. In addition, there are significant considerations regarding privacy, data ownership, and the psychological implications of disclosing genetic risks to patients.
Transforming VUCA Challenges into Opportunities
While the VUCA framework depicts intricate challenges in healthcare, it also paves the way for positive transformation. By viewing volatility as an opportunity for innovation, uncertainty as a catalyst for strategic foresight, complexity as a driver for multidisciplinary collaboration, and ambiguity as a trigger for creative problem-solving, healthcare organizations can thrive even in this tumultuous VUCA environment.
Let’s now look at each component, exploring how these obstacles can be transformed into actionable strategies for growth.
Volatility, while initially perceived as a hurdle, can fuel the fire of innovation. For instance, the volatility in health policies and regulations, often regarded as a hindrance, can allow organizations to develop agile response strategies. This agility becomes a competitive advantage, enabling faster adaptation to changes and maintaining stability in unstable times.
Imagine a healthcare organization with a built-in flexible policy adaptation model. It allows for rapid response and adaptation to any new healthcare guidelines or regulations, ensuring that care delivery is always compliant, safe, and effective. This nimble approach could reduce the time and resources spent implementing new guidelines and potentially improve patient satisfaction and outcomes.
Uncertainty about disease outbreaks or the evolution of patient needs can inspire the creation of proactive surveillance systems. These systems, driven by AI and predictive analytics, can bolster healthcare’s preparedness and response mechanisms.
Consider a system that collects and analyzes data from multiple sources – electronic health records, social media, weather reports, and more – to predict potential disease outbreaks. Such a system could enable healthcare organizations to better prepare for outbreaks, ensuring they have the necessary resources and can quickly implement response strategies.
Complexity, particularly in chronic disease management, can stimulate the development of coordinated care models. A complex condition like diabetes requires a multidisciplinary approach involving primary care physicians, endocrinologists, nutritionists, and more. Healthcare organizations can develop models that promote collaboration across different care professionals by viewing this complexity as an impetus.
Think of a diabetes patient’s treatment involving a mobile app allowing real-time communication between the patient and all healthcare providers involved. This model fosters collaboration and ensures that the patient is at the center of all decisions, thereby improving health outcomes.
Ambiguity, often found in genetic testing interpretations, can provoke a shift toward patient-centered decision-making. Rather than viewing ambiguity as a challenge, it can be seen as an invitation for shared decision-making and personalized care.
For example, consider a scenario where a patient’s genetic test reveals a predisposition for both heart disease and diabetes. Instead of a one-size-fits-all approach, clinicians and the patient can engage in shared decision-making, considering the patient’s lifestyle, preferences, and values to decide on the best preventative measures.
Measuring Transformational Success in the VUCA Landscape
The success of the VUCA strategy is measurable, reflected in Key Performance Indicators (KPIs) such as improved health outcomes, reduced health disparities, enhanced operational efficiency, and financial sustainability. For instance, using the VUCA strategy, healthcare organizations can reduce readmission rates—a key indicator of healthcare quality and efficiency. Creating coordinated care models can ensure patients receive appropriate post-discharge care, thereby reducing readmissions.
Improved Health Outcomes: Consider the metric of patient readmission rates, a key barometer of healthcare quality and efficiency. By employing a VUCA-responsive strategy, healthcare organizations can significantly reduce these rates. For instance, an acute care hospital may implement a comprehensive care transition program to support patients post-discharge. This program may involve a team of care coordinators, social workers, and community health workers who connect with patients after discharge, ensuring they understand their medications, follow-up appointments, and available community resources. By this concerted approach, the hospital can significantly decrease the readmission rates, thus reflecting improved patient outcomes.
Diminished Health Disparities: Another measure of VUCA strategy success can be seen in reduced health disparities. Consider a public health department that uses predictive analytics to anticipate and address health disparities. By analyzing demographic data, social determinants of health, and health outcomes, they can target resources effectively to vulnerable communities. For instance, if data analysis reveals a higher incidence of hypertension in a specific community, the department can initiate targeted interventions such as community education, blood pressure screening events, or improved access to care in those areas. As a result, the health department can measure its success by the reduced rates of hypertension and related complications in the targeted communities.
Enhanced Operational Efficiency: Operational efficiency is another critical KPI demonstrating VUCA strategies’ efficacy. Consider a healthcare organization that adopts an electronic health record (EHR) system to streamline patient data management. Through effective training and implementation, the organization can see reduced data retrieval times, less duplication of tests, and improved coordination among healthcare providers. Consequently, the success of this VUCA strategy can be measured by the increased operational efficiency reflected in the improved metrics.
Financial Sustainability: Financial sustainability is a tangible measure of successful VUCA strategy execution. An example could be a community clinic that adopts a value-based care model. This model emphasizes preventive care and managing chronic conditions to avoid expensive hospitalizations and complications. The clinic could track metrics like the cost of care per patient and the number of emergency department visits. A decrease in these metrics would signify financial sustainability, indicating that the clinic’s VUCA strategy is successful.
Setting Sail in Healthcare’s VUCA Sea
Despite the inherent complexities and challenges, healthcare organizations can successfully navigate the VUCA landscape by employing strategic leadership, innovative tools, and collaborative approaches. In doing so, healthcare leaders can transform their organizations into agile, resilient, and patient-centric entities capable of delivering equitable, high-quality care. The journey may be turbulent, but they can set sail confidently toward their destination with a strategic blueprint.
How We Help You Navigate VUCA
At ORET Healthcare, our innovative 3×3 approach is specially designed to steer healthcare organizations through the turbulent waters of VUCA. This approach integrates data analytics, Lean Six Sigma methodology, and cutting-edge technology to confront challenges in healthcare’s clinical, financial, and regulatory dimensions.
Data analytics extracts critical insights from complex health data, fostering evidence-based decision-making. Lean Six Sigma methodology is implemented to streamline processes and reduce waste, optimizing your operations. Technology solutions, the third pillar, encourage the integration of digital transformations like telehealth services and AI, fostering an agile and adaptive organizational environment. Through ORET Healthcare, you gain a partner that enables survival and success in the challenging VUCA landscape.
